The Basics for Food Allergies
Food Allergy Facts
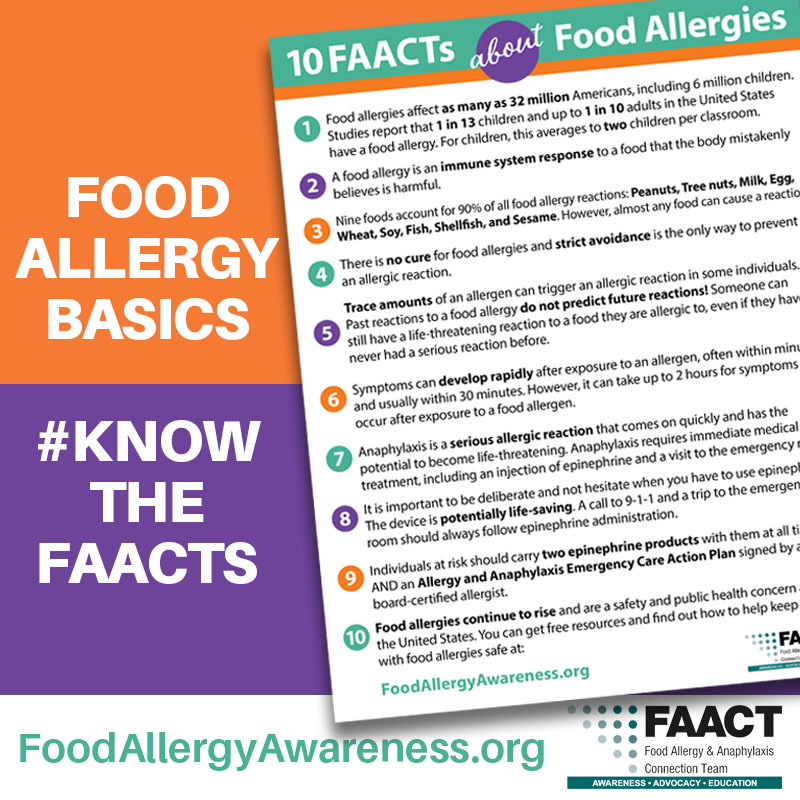
Prevalence:
- Food allergies affect as many as 32 million Americans, including 26 million adults and 5.6 million children.
- Approximately 7.6% of children and 10.8% of adults in the United States have food allergies.
- Food allergies are more prevalent in children than in adults, but many affected children can "outgrow" food allergies with age (CDC).
- The prevalence of food allergies in children increased by 50% between 1997 and 2011 (CDC).
- Among children under 18, it is common enough that there are about 2 students with food allergies in every classroom.
Immune System Response:
- A food allergy is an immune system response to a food the body mistakenly believes is harmful.
- When a person with a food allergy eats the food, the immune system releases massive amounts of chemicals, including histamine, triggering symptoms affecting the respiratory system, gastrointestinal tract, skin, and/or cardiovascular system.
Management and Risks:
- There is no cure for food allergies.
- Food allergy desensitizations are being studied but are not yet proven treatments.
- Strict avoidance of allergens is the only way to prevent an allergic reaction.
- Managing a food allergy daily involves constant vigilance.
- Even trace amounts of an allergen can trigger an allergic reaction in some individuals.
- Food allergy deaths can occur, even among those with a history of mild reactions in the past.
- In case of an anaphylactic reaction, 9-1-1 must ALWAYS be called.
What is Anaphylaxis (an–a–fi–LAK–sis)?
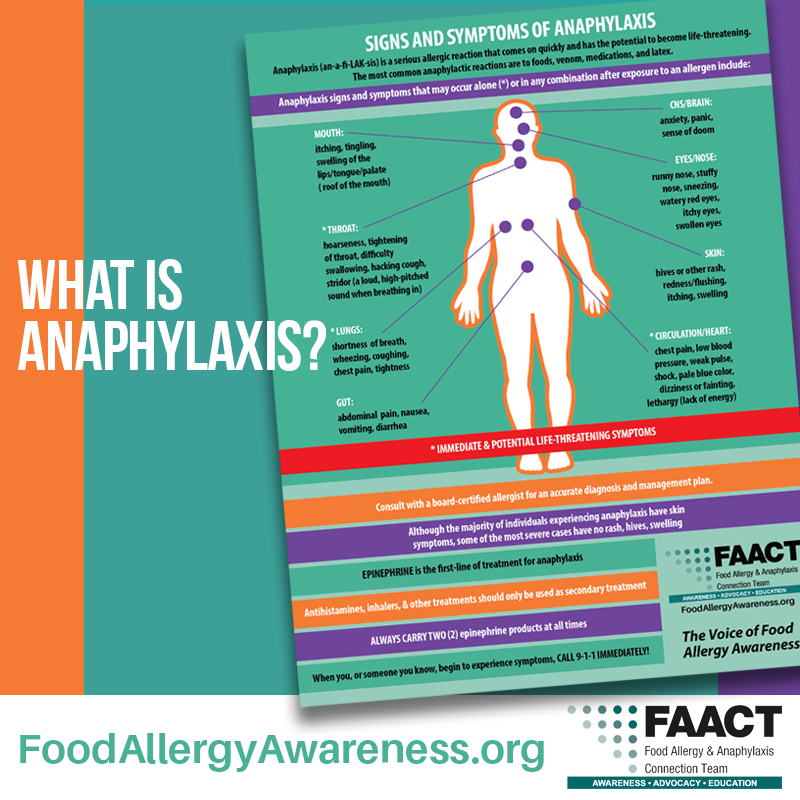
Anaphylaxis Definition:
- Anaphylaxis is a serious allergic reaction that comes on quickly and has the potential to become life-threatening.
- It can be triggered by food, latex, insect stings, and medicines.
Symptoms and Onset:
- Symptoms can develop rapidly, often within minutes, and usually within 30 minutes after exposure to an allergen.
- For food allergens, symptoms can take up to 2 hours to appear.
- Signs and symptoms of anaphylaxis can occur alone or in combination.
Immediate Action Required:
- Anaphylaxis requires immediate medical treatment, including the administration of epinephrine and a visit to the emergency room.
- Prompt administration of epinephrine is crucial to surviving a potentially life-threatening reaction. Epinephrine has very few side effects and is available as an auto-injector device (Auvi-Q®, EpiPen®).
- Anaphylaxis can be fatal if not treated promptly.
Post-Reaction Care:
- Observation in a hospital for 4 to 24 hours is recommended after the individual returns to normal due to concerns of biphasic anaphylaxis.
- Biphasic anaphylaxis is a second round of allergic reactions that can occur after the initial reaction. It may happen as early as an hour or 72 hours later, with an average of 10 hours. This second reaction can be less severe, as severe, or even more severe than the initial reaction.
Preparation for At-Risk Individuals:
- If you or someone you know is at risk of anaphylaxis, carry two epinephrine auto-injectable devices.
-
Prompt administration of epinephrine is crucial to surviving a potentially life-threatening reaction. Epinephrine has very few side effects; auto-injector devices include Auvi-Q®, EpiPen®.
Statistics in the U.S.:
- Each year, severe reactions to food cause:
- 30,000 emergency room visits
- 2,000 hospitalizations
- 150 deaths

Nine Foods Account for 90 Percent of All Food Allergy Reactions:
- Peanuts
- Tree nuts (cashews, pecans, walnuts, etc.)
- Milk
- Egg
- Wheat
- Soy
- Fish (halibut, salmon, etc.)
- Shellfish (crab, lobster, shrimp, etc.)
- Sesame
While more than 170 foods can cause allergic reactions in people with food allergies, the law identifies the nine most common allergenic foods (4).
For FREE and downloadable resources, visit:
FAACT's Living with Food Allergies Resource Center
To learn more about food allergy, we recommend this video by the National Institute of Allergy and Infectious Diseases:
"Understanding Food Allergy"

When It Comes to Food Allergy Safety, It’s a Matter of FAACT!
Food Allergies are REAL and can be FATAL! Anaphylaxis is a serious allergic reaction that comes on quickly and has the potential to become life-threatening.
Avoiding Allergens is a MUST! Never assume something is safe - ALWAYS read ALL labels for their ingredient and manufacturing information.
Allergies to Food are NOT a joke! NO child should ever be bullied, teased or excluded, especially due to their food allergy.
Cross-Contact CAN happen! Proper cleaning of hands, cookware, utensils, and also surfaces is vital for preventing exposure to allergens.
Together, We CAN Make a Difference! FAACT is here to provide support and helpful resources that you can easily learn, print, and share!
Download 'Food Allergy Safety, It's a Matter of FAACT' poster
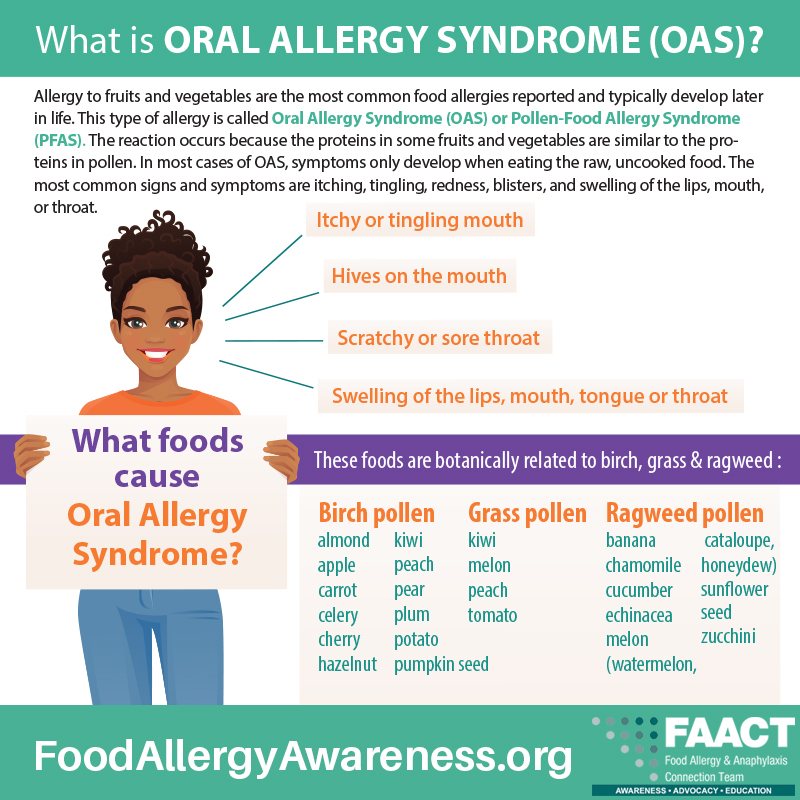
Oral Allergy Syndrome
Allergy to fruits and vegetables are the most common food allergies reported by adults and typically develop later in life. This is called Oral Allergy Syndrome (OAS) or Pollen-Food Allergy Syndrome (PFAS)—a reaction that occurs because the proteins in some fruits and vegetables are similar to the proteins in pollen.
In most cases of OAS, symptoms only develop when eating the raw, uncooked food. The most common symptoms are itching, tingling, redness, blisters, and swelling of the lips, mouth, or throat.
A Food Allergy is NOT:
- A food intolerance (lactose intolerance, gluten intolerance, etc.).
- An intolerance does not involve the immune system – it involves the digestive system because the body lacks an enzyme needed to digest and process a particular food.
- Symptoms of an intolerance include gas, bloating, and abdominal pain.
- A food preference (vegetarian, kosher, etc.).
- Celiac Disease (is a NON-IgE mediated food allergy).
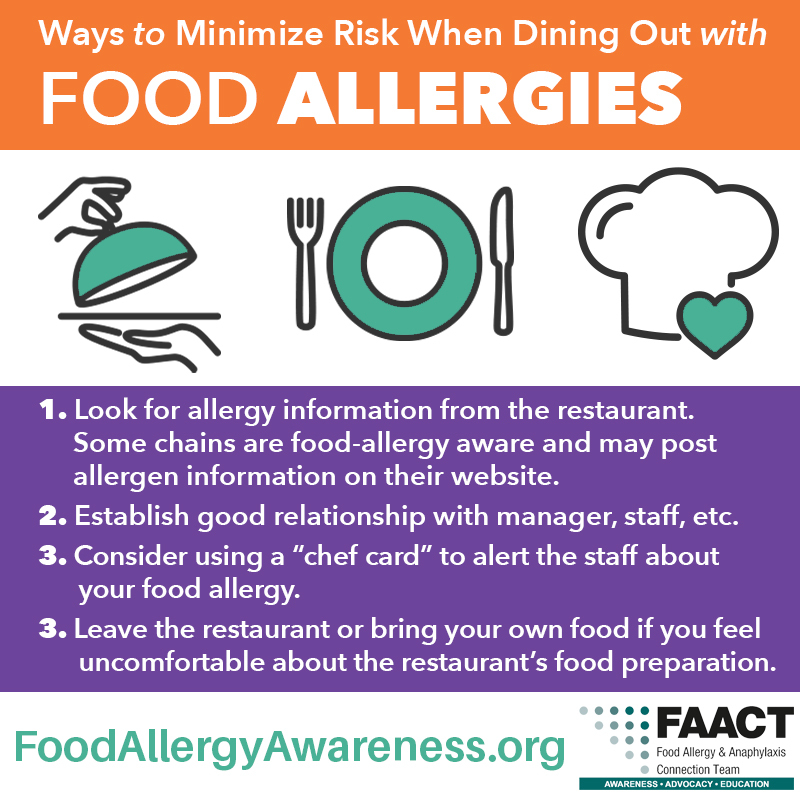
Minimize Risk When Dining Out with Food Allergies
There are ways to minimize risk of accidental exposures and feel more secure about eating out.
- Look for allergy information from the restaurant. Some chains are food-allergy aware and may post allergen information on their Web site.
- Establish good relationship with manager, staff, etc.
- Consider using a “chef card” to alert the staff about your food allergy.
- Leave the restaurant or bring your own food if you feel uncomfortable about the restaurant’s food preparation.
For more information about food allergies and FREE downloadable resources, visit FAACT's Living with Food Allergies Resource Center
Tips for Preparing to Dine Out
Reduce Your Risk!
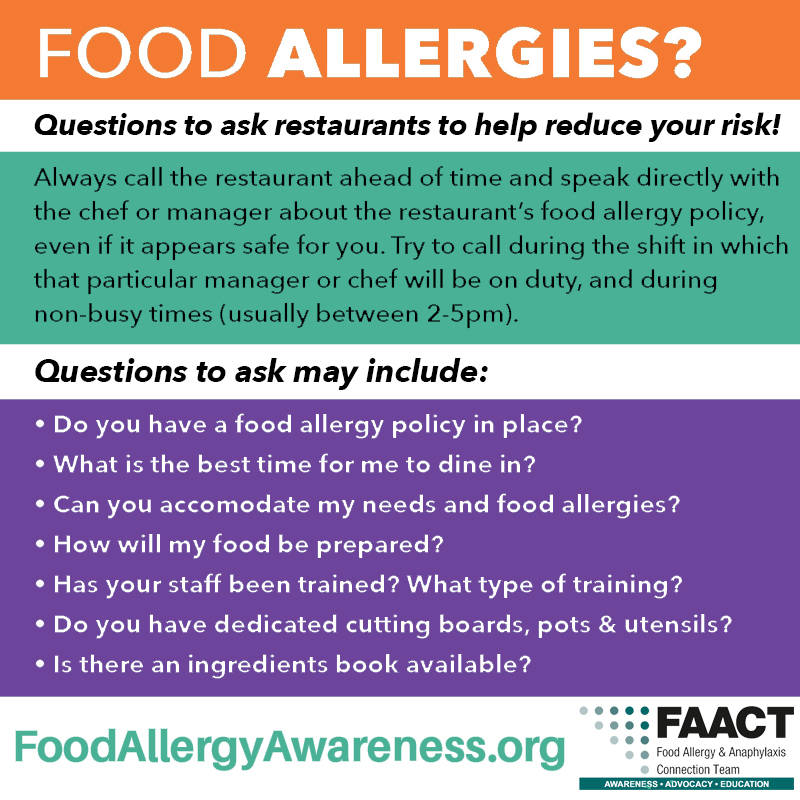
- Always call the restaurant ahead of time and speak directly with the chef or manager about the restaurant’s food allergy policy, even if it appears safe for you. Try to call during the shift in which that particular manager or chef will be on duty, and call during non-busy times (usually between 2pm-5pm). Questions to ask may include:
- Do you have a food allergy policy in place?
- Can you accommodate my needs and food allergies?
- How will my food be prepared?
- Have your staff been trained on food allergies? What type of training?
- Do you have dedicated cutting boards, pots, and utensils?
- Is there an ingredients list available?
- Avoid dining during busy times (e.g., dinner rush, holidays, after church, and weekends).
- Compile a list of questions to ask before you go.
- Upon arrival, inform the hostess and server of your allergens and ask to speak to the manager on duty. Wipe down your seats, the table, and menus with a hand wipe.
- Order simple foods. Dishes with sauces or that are cooked on the grill or in the fryer can increase your risk for cross-contact with allergens.
- Avoid high-risk situations, including:
- Buffets, self-serve shops, and deli stations (cross-contact risk).
- Bakeries and ice cream shops (cross-contact risk).
- Restaurants with a heavy concentration of your allergen.
- Pizza or sandwich shops (cross-contact risk).
- Events and venues serving ingredients you are not familiar with.
- Events or venues that may present barriers to effective communication due differences in language (cards are available in many languages from Equal Eats).
- Ways to minimize risk when dining out with food allergies:
- Look up allergy information online. Some chain restaurants post detailed allergen information on their websites.
- Communicate clearly and often while asking critical questions.
- Use a chef's card to communicate your allergies to servers and kitchen staff (cards are available in many languages from Equal Eats).
- If you don't feel comfortable with food preparation, leave the restaurant politely.
- Always carry your prescribed medications and act quickly in the event of an emergency! Know the "Signs and Symptoms of Anaphylaxis."
- If a mistake is made, keep the dish at your table rather than have the staff return it to the kitchen. Once the new dish has been prepared properly, you can return the old dish. This will ensure that the allergen was not just "removed."
- Prepare for the unexpected. Pack a small snack in case the restaurant is not able to cater to your needs.
References
4. Boyce JA, Assa’ad A, Burks AW, et al; NIAID-Sponsored Expert Panel. Guidelines for the diagnosis and management of food allergy in the United States: report of the NIAID-sponsored expert panel. J Allergy Clin Immunol. 2010;126(suppl 6):S1-S58. Available at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4241964/

